In 2014, Jason Mendelsohn was 44, had recently lost weight through Weight Watchers, and was feeling the most fit he’d ever been in his life. He had three kids, a wife of 17 years, and was the president of his family’s insurance company.One day, while taking a financial services exam for his business, he rested his head in his hand to ponder a test question when he felt a dime-sized lump on his neck. “All of a sudden, I get a cancer diagnosis,” he tells me, describing the weeks that followed. “I’m like, are you kidding me? I had never even contemplated that I might get cancer because I felt so good, and literally had no symptoms.” Mendelsohn was diagnosed with stage 4 oropharyngeal cancer, or cancer of the head, neck, or throat.
Advertisement
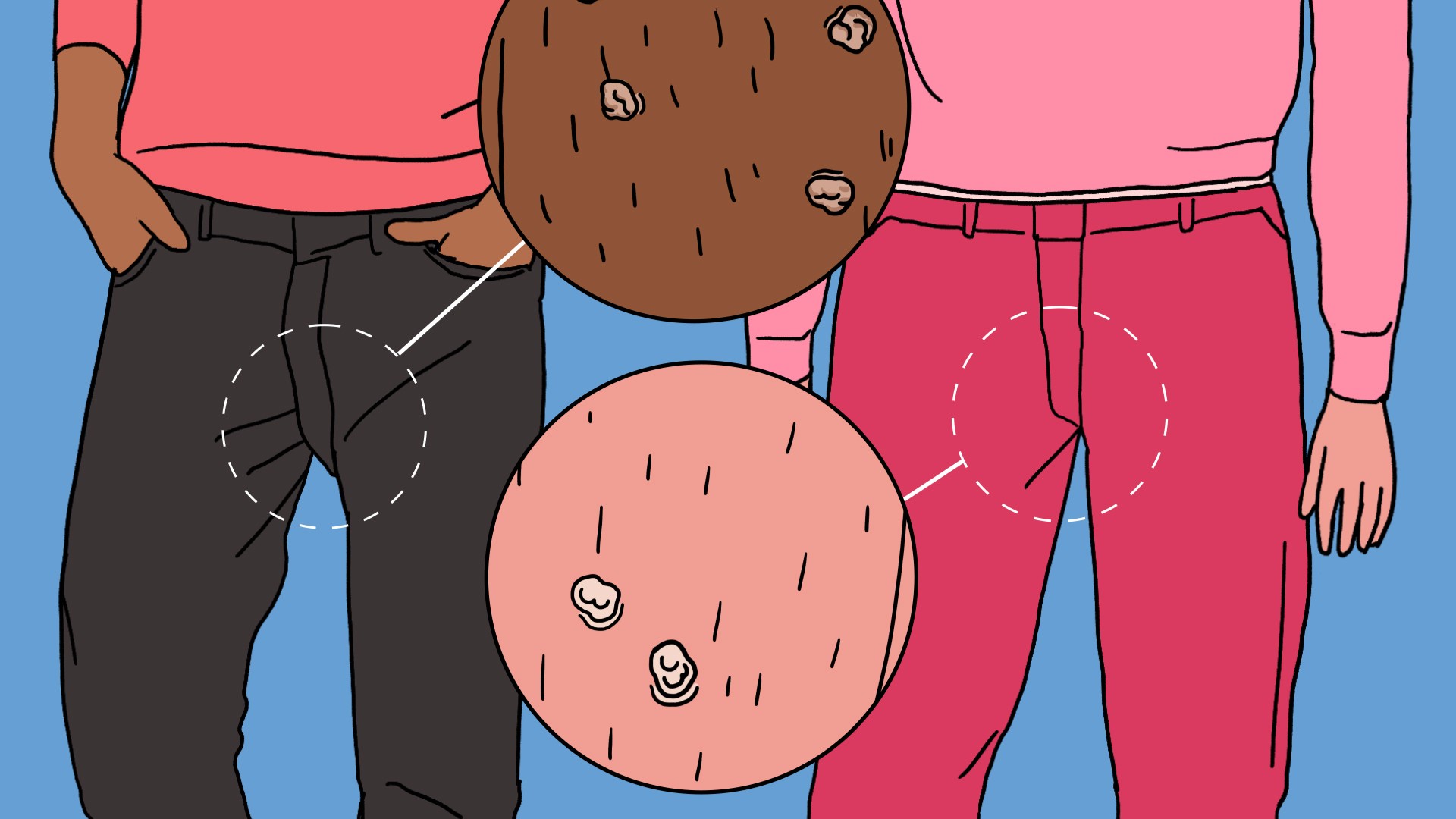
In the past, Mendelsohn wouldn’t have been a typical candidate for this kind of cancer. “Physicians were used to older patients with smoking or drinking history,” says Carole Fakhry, a head and neck surgeon at Johns Hopkins Medicine.But over the past decades, doctors have been seeing an influx of younger men with head and neck cancers, often non-smokers, and otherwise in good health—until they noticed that lump in their throat. Rates of oropharyngeal cancer among men have been steadily rising, more than 300 percent in the past 40 years. The cause? Human papillomavirus, or HPV.A study from last year found that one in nine men ages 18 to 69 were infected with oral HPV. That’s 11 million men, compared to 3 million women. Not all HPV carries a cancer risk, but the strain that does, oral HPV 16, was six times more common in men than women in the study.And while the knowledge of HPV-related cancers in men is gradually becoming better-known—partly because of its increasing prevalence—doctors are still learning new things about the characteristics of the cancer itself.“For decades we would say head and neck cancer, particularly in its advanced stages, has a relatively poor outcome,” says Eric Moore, an otolaryngologist and surgeon at The Mayo Clinic. According to Moore, people with traditional head and neck cancer will eventually die from that cancer 50 percent of the time—even with treatment.
Advertisement
"But, this cancer behaves so much differently than that," he says. "For the most part, about 90 percent of the people who develop HPV-related tonsil- and tongue-based cancer will survive their cancer and be cured with treatment. It’s such a drastic difference, it’s changed the whole way we think about this particular cancer, how people are going to live after their treatment, and what the long-term side effects of that treatment going to be.”Many aspects of HPV-related cancer in men have taken a different publicity route to similar cancers in women. In the 1980s, Scandavian medical studies highlighted the relationship between HPV and uterine cervical carcinoma, leading to yearly pap smears, HPV education for women, and eventually the HPV vaccine. But around the same time, a Finnish group wrote an article about how there were similarities in some head and neck cancers, too.“It just didn’t catch on,” Moore says. “Nobody ran with, and it kind of died.” It wasn’t until 24 years later that the subject got attention when a 2007 study from a small Colorado Springs ear, nose, and throat practice noted the rising incidence of cancer and the role of papillomavirus.“It wasn’t rapid, like over one year we saw something very different,” Moore says. “It was so gradual that it took a while to catch on and recognize it for most people. But personally, in our own clinic, it’s become the most common surgical cancer that we treat.”
Advertisement
How does a virus cause cancer? Viruses can’t make copies of themselves, instead, they hijack the reproductive machinery of cells to do the job. Eventually, the cell will die, leaving the virus without a way to reproduce. One way to get around that is to "re-wire" the cell to live and reproduce forever. “And a cell that’s making infinite copies of itself is a cancer cell,” Moore says.Tumors caused by HPV express different proteins on their surface, and doctors can test those cells when they take biopsies to see if the tumor is related to the virus. Moore says it’s crucial to get these cancers tested for HPV, because he and others have been learning how differently HPV-related oropharyngeal cancers respond to treatment. At Mayo, he’s been slowly and methodically de-escalating or de-intensifying treatments with informed consent from his patients.One patient that Moore treated was a pregnant woman in her second trimester. She couldn’t have chemotherapy or radiation therapy, which are normally standard for oropharyngeal cancer. Moore knew that her cancer was caused by HPV and treated her with surgical removal of her tumor only, and monitored her progress closely. That was almost a decade ago, he says, and she's still cancer-free.
Watch more from TONIC: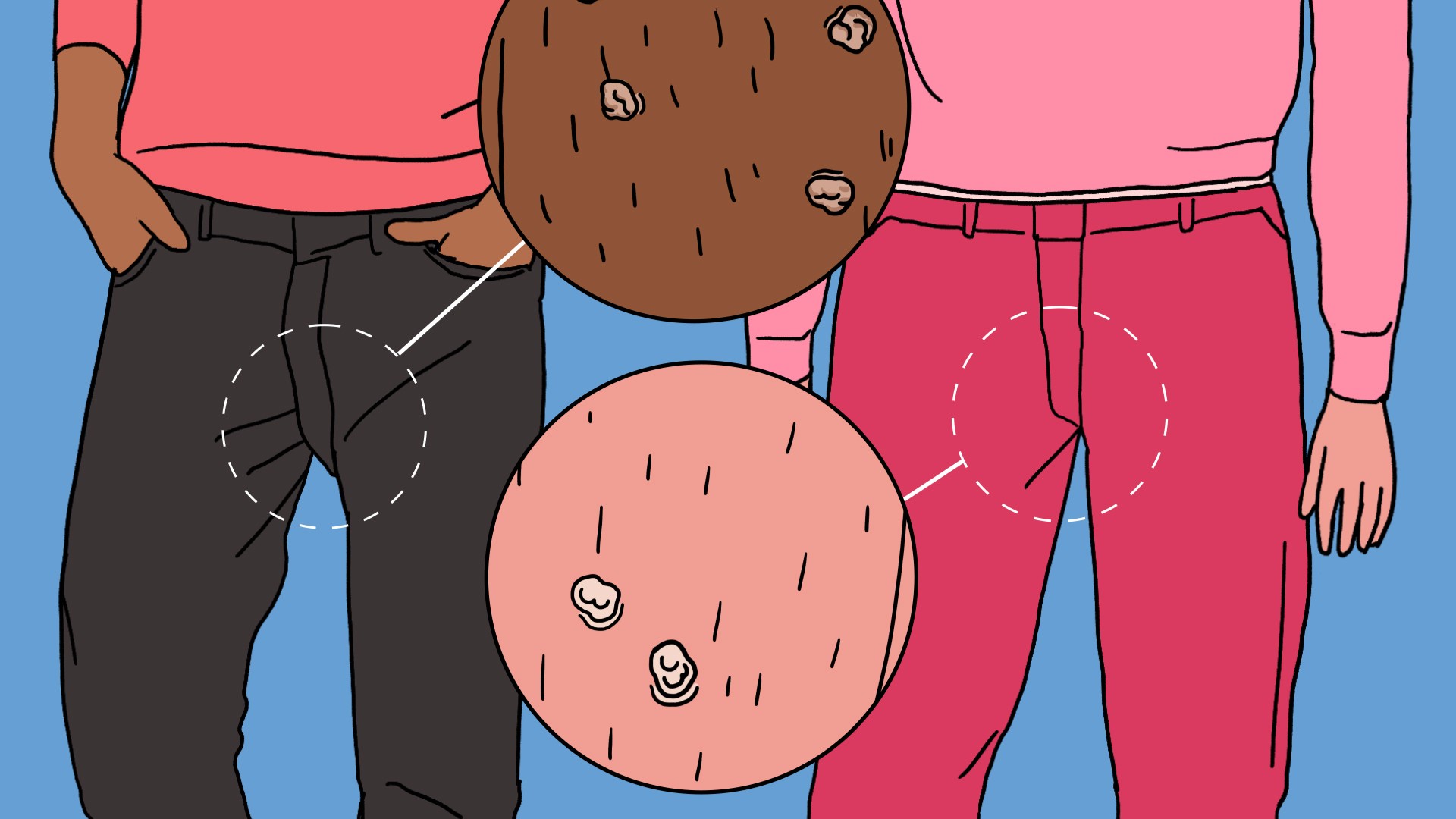
Moore says doctors are realizing that many cases might be successful with surgery only, or combining surgery with about two weeks of radiation. In traditional head and neck cancer, radiation would typically be given for six or seven weeks, plus surgery, with an optional side of chemotherapy.
Watch more from TONIC:
Moore says doctors are realizing that many cases might be successful with surgery only, or combining surgery with about two weeks of radiation. In traditional head and neck cancer, radiation would typically be given for six or seven weeks, plus surgery, with an optional side of chemotherapy.
Advertisement
That’s what Mendelsohn endured, saying that at the peak of his radiation treatment, he stayed in bed for 18 hours a day. It’s possible he would have received less treatment if he was diagnosed today—even the stage of his cancer might have been different. Beginning on January 1 of this year, there is now a separate staging algorithm for HPV-related cancer of the head, neck, throat and surrounding areas, distinguishing it from typical oropharyngeal cancer because of how different the treatments and outcomes could potentially be.Mendelsohn tells me that, with his same biopsy results from 2014, he wouldn't have been classified as stage 4 today. Instead, his doctor recently told him his cancer would have been stage 1.Moore says cancer treatments take a long time to change, and for good reason—doctors need to make sure they’re effective. Researchers don’t definitively know why HPV-related head and neck cancer is more treatable and less likely to spread to other parts of the body, but Moore says there are a few theories.One is that the immune system may have more fighting power against a virally induced cancer. There’s evidence that people who have compromised immune systems from HIV or anti-rejection organ meds have a higher chance of getting cancer, and having more aggressive cancers. “Maybe because the immune system is primed throughout the eons to combat viral infections?” Moore says. “Maybe that’s why these tumors respond so well because the immune system can target and find them very easily.”
Advertisement
Also, carcinogens like cigarette smoke and alcohol often cause traditional head and neck cancers. Those exact a lot more DNA damage than the viruses do, and Moore says that treatment might be harder when tissue is so damaged. (Papillomaviruses change a smaller amount of DNA of cells in a very specific way.)“The other thing that’s interesting, is that [those changes are] reversible,” Moore says. “So the papilloma virus doesn’t destroy the DNA, it just produces proteins that kind of turn [things] off. When you get rid of those proteins and the papillomavirus, those things reverse. So it’s maybe just a less lethal cancer.”These theories reinforce the message that Moore wants broadcasted far and wide: make sure your doctor checks your oropharyngeal head, neck or throat cancers for HPV. “This is not common knowledge at all,” he says. “You think, 'Well this has been going on for 10 years.' But dissemination of knowledge and rapid recognition and things like that don’t just happen automatically in medicine, unfortunately.”It’s currently recommended to check all head and neck cancers for HPV, but it’s not as widespread as some doctors would like. “It is now expected that all oropharyngeal cancers be tested for HPV but I still see the majority of my patients, who come from many states, that did not get their cancer tested,” says Terry Day, director of the head and neck tumor center at the Medical University of South Carolina.
Advertisement
There also isn't a good general screening tool to check for HPV. Cheek swabs can only test for HPV in general, and aren’t as good at finding high-risk HPV. Even if there was a good test, most people who get high-risk HPV won’t develop cancer, so any such test might raise false alarms.It's a good thing, then, that we have a vaccine. The HPV vaccine that's already available to us has been shown to be effective in protecting against oral cancers, too. Moore says that while the vaccine was designed for younger children, we don’t know for sure that adults won't also benefit from it. In the off chance you haven’t been exposed to HPV, it could protect you from cancer, whether you’re a man or woman. The HPV vaccine recommendations are finally extended to include girls and boys, but the number of boys receiving it is much lower. Parents of boys may have to specifically ask for it, and Day tells me that his insurance didn’t cover his son’s vaccine, and he had to pay out of pocket for it.“This cancer has changed more rapidly than any other type of treatment or cancer that we treat and I think it’ll still continue to evolve,” Moore says. “Hopefully we’ll someday wind up with a disease that we know how to treat with very little treatment. And hopefully someday we’ll find a way to make sure that everybody’s vaccinated against it and they won’t get this cancer.”Mendelsohn has been cancer-free for three years, and is devoted now to HPV cancer and vaccine advocacy. Though it’s possible he could have received a different treatment plan, at the time he wanted to do everything he could to ensure he survived, he says. His goal isn't to lament the past, but to spread the message about his cancer to help others avoid the same uncertainty.“I had no idea if I was going to live,” he says. “A month in, I made videos to each of my three kids that said, 'One day you’re going to get married, I’m not going to be there, this is what’s important.' So what drove me over the last few years to go public was hopefully stopping any other father or mother from ever having to make videos to their kids, similar to what I did.”Read This Next: 8 Things People Still Get Wrong About HPV
